While last year had many challenges, it also catapulted the evolution of healthcare payments and communications. From high rebates to a drop in member satisfaction with communications, the industry dealt with unprecedented challenges that forced it to adapt. With lower claim volume, payers have had to pay large rebates to customers due to MLR (Medical Loss Ratio) requirements.
The increase in laid off and furloughed employees has resulted in a membership transition from commercial plans to Medicaid and self-pay. Payers need to find a better way to reduce costs and keep members and providers happy. Members are confused by the large volume of transactional claim communications and want to better understand what they owe. That’s where the shift towards electronic payments and episodic communications comes in.
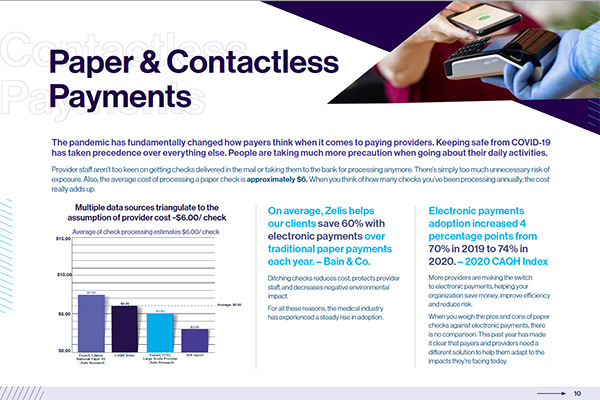
$450B in paper check payments still exists today across providers.
— Bain & Company
Getting your providers to make the switch from paper checks to electronic will help streamline operations and unlock the next level in efficiency.
Giving your members clearer, more concise communications helps improve visibility into their healthcare claims.
“Clearer EOB’s have improved member satisfaction and faster electronic payments have increased provider satisfaction.”
— MA Health Plan COO
This guide will help you drive savings and increase efficiency. It will give you the insights you need to optimize your payments and communications process in 4 simple steps.