Whether you need a first-pass editor or a secondary one, Zelis Claims Editing fits in your workflow to ensure you are capturing the most savings possible.
Healthcare Claims Editing with Zelis.
Proactively identifying billing errors is proven to reduce overpayments and provider abrasion, all while improving savings. That’s why we examine every claim using a combination of a growing library of edits, historical data, industry knowledge, and the expertise of a team of certified professional coders, registered nurses, and medical doctors.
Dive Deeper
Improve payment accuracy with a holistic approach.
Optimize revenue opportunities with expert analysis and recommendations on your claims payments and trends, reducing claim appeals with adherence to coding standards. Zelis Claims Editing is designed to fit your claims processing and payments workflow where you need it. Our out-of-the box approach provides a flexible solution that ensures timely, accurate payments.
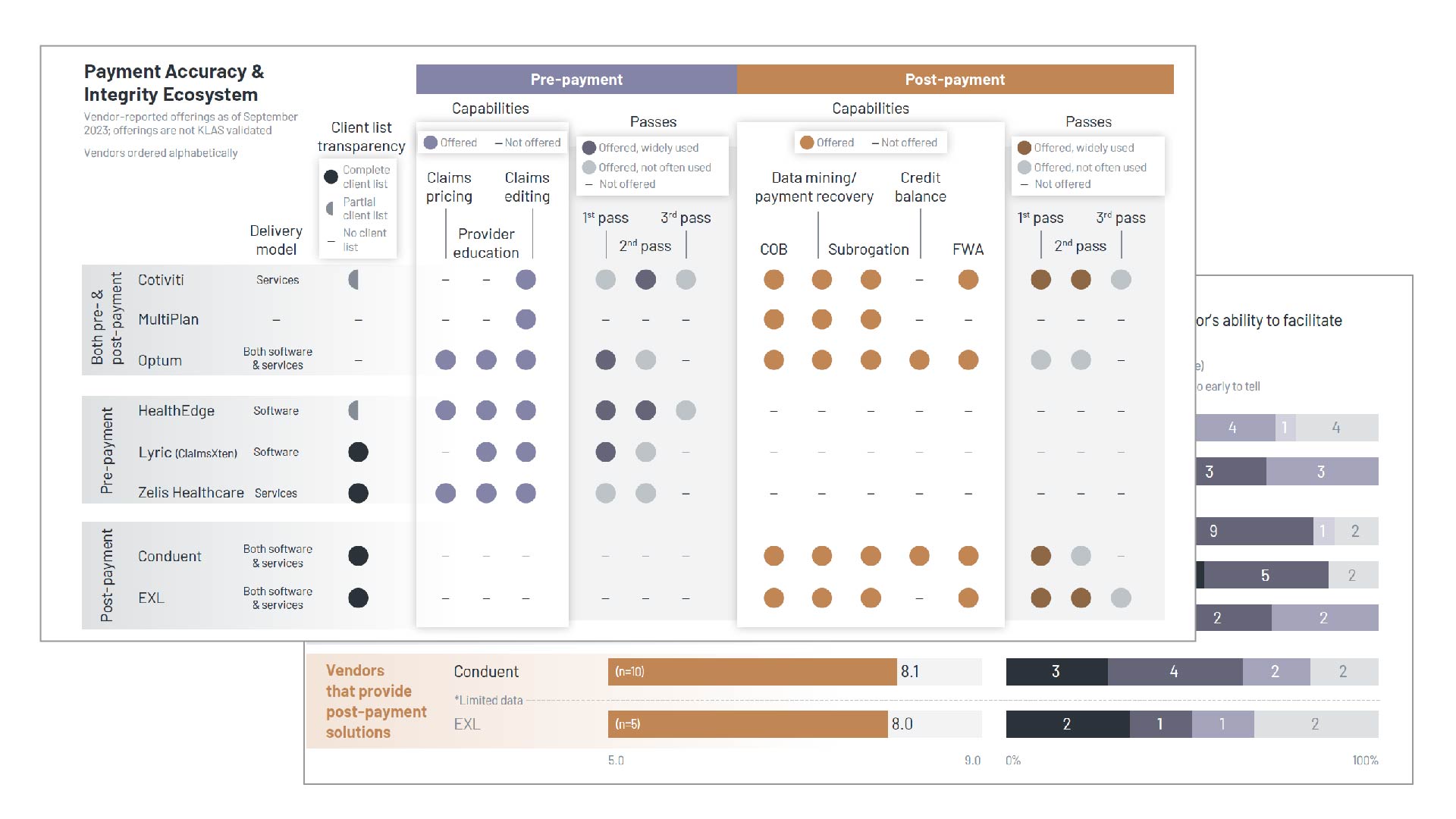
Leading Performer in 2023 KLAS inaugural Payment Accuracy & Integrity Solutions Report
KLAS, a leading independent healthcare analyst firm, recently profiled 8 Payment Integrity vendors through hours of direct customer interviews, vendor briefings, and market insights. The result is a comprehensive view of the payer payment integrity landscape, and Zelis is the top-rated vendor.
Read the ReportBy the Numbers
Measurable savings on every claim.
0
of Zelis claims edits are disputed
0
of Zelis claim edits are reversed
Our relationship with Zelis has given us the flexibility to create customized solutions and bring value to our clients. The solutions and expertise that Zelis brings to the table, as well as its team’s ability to develop ideas to improve our processes, have created a mutually beneficial relationship for both our companies.
Our team recommends Zelis to any third-party administrators that are seeking a partner that will help them deliver superior service, provide strong cost reduction solutions, and continually looks for ways to improve its products and services.
Zelis has always given us the tools we needed to succeed. Working with their team has helped us navigate the constantly changing demands of the market that are generated by our clients’ needs, regulatory issues, and the passage of new legislation. We have a level of confidence that when something new comes up, we’re going to work with Zelis to solve the problem.
Request a Meeting
Let’s talk about modernizing your business.
There’s no shortage of ways we can help. Get a conversation going with one of our Solution Advisors and build a thoughtful approach aligned to your business goals.
Not what you were looking for?



