Remarkable service from remarkable people who have been in the trenches before. Whether that’s in the OR, the front-lines of the ER, or hands-on in more specialized units, our expert billing and coding team is here to design, build and support solutions just for you.
Expert Claims Review with Zelis
Fortify your payment integrity operations with a bill review solution built by healthcare experts. Bringing remarkable service from remarkable people to our pre-pay bill review offering, we offer a solution built for your reality.
Dive Deeper
Improve savings with multi-layer bill review.
Bill review was once something that healthcare payers could ‘set and forget,’ but those dynamics have shifted. Payers must now fight competing pressures: balancing cost of care for both members and providers, all while navigating ecosystem-wide pressures driven by thinning margins and evolving regulations. The complexity is greater, and the stakes are higher.
Uncover coding errors and inappropriate charges with expert, end-to-end claims review by a team of experienced clinicians (including nurses, physicians, pharmacists and more) and certified coders that review inpatient, outpatient and professional higher dollar medical claims to ensure claim payment accuracy and improve savings on your costly claims.
Our comprehensive pre- and post-payment approach uses itemized bill review, clinical chart review, and diagnoses related groups (DRG) validation to focus on billing compliance, cost analysis, financial outliers, and adherence to plan policies and billing standards.
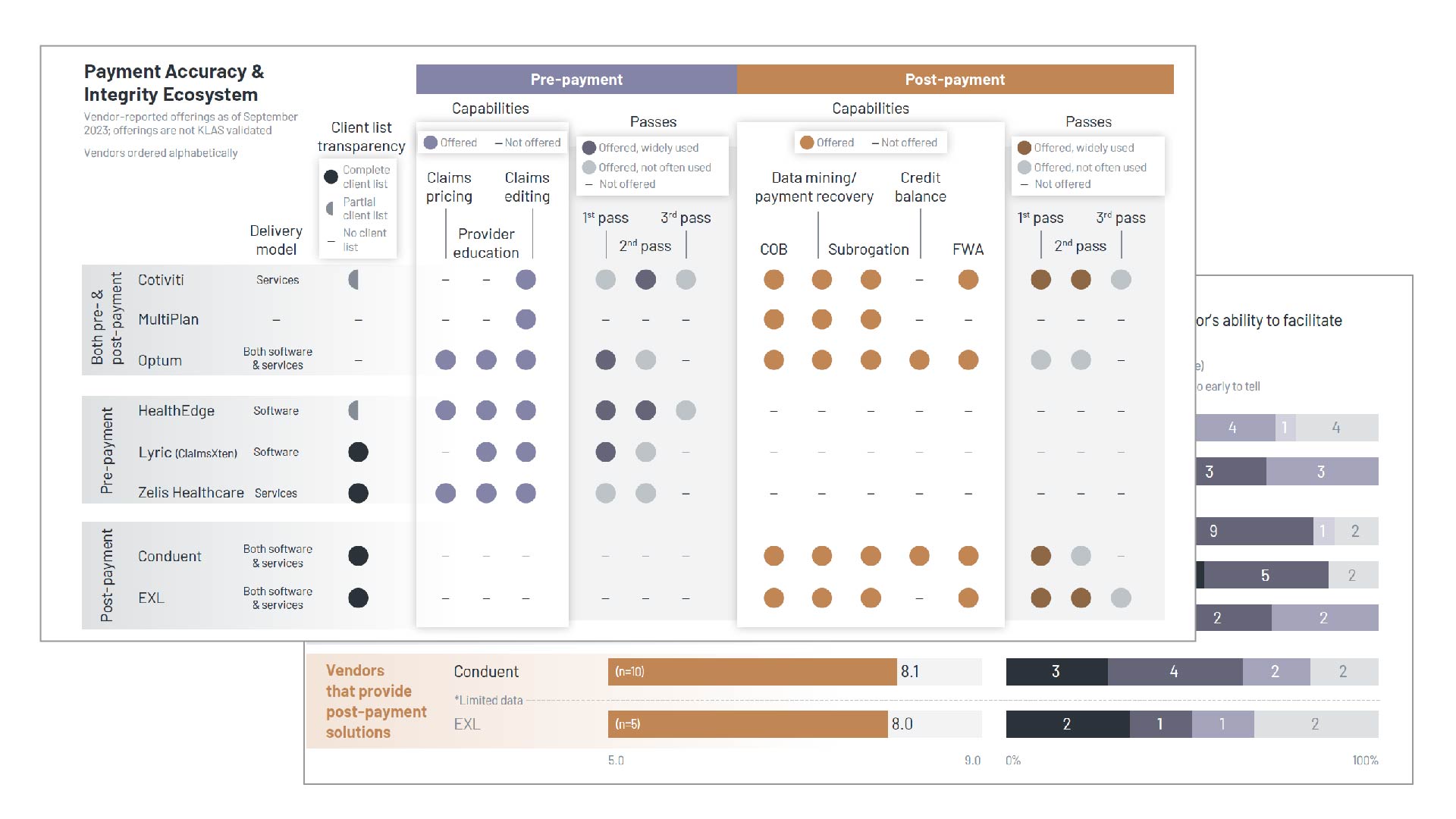
Leading Performer in 2023 KLAS inaugural Payment Accuracy & Integrity Solutions Report
KLAS, a leading independent healthcare analyst firm, recently profiled 8 Payment Integrity vendors through hours of direct customer interviews, vendor briefings, and market insights. The result is a comprehensive view of the payer payment integrity landscape, and Zelis is the top-rated vendor.
Read the ReportA Suite of Solutions
Expert Claims Review Capabilities
Line-by-line review of complex claims leveraging the best of human expertise and advanced technology to identify incorrect coding and billing errors that often contribute to overpayments and decreased savings.
Clinical review of the itemized bill and medical record to identify clinical inaccuracies and ensure the claim was billed appropriately according to the payers’ medical policies, including reviews of high-cost drugs.
Clinical or financial review of claims paid by either APR or MS-DRG reimbursement methodologies in either Medicare, Medicaid, or Commercial business lines to ensure compliance and accuracy in claim payment.
Comprehensive claim review to ensure deepest level of savings on high-cost out of network or full benefit carve dialysis claims for self-funded plans providing upwards of 90% of savings through our proprietary reimbursement and support approach.
By the Numbers
Measurable savings on every claim.
0
average savings rate per claim for Itemized Bill Review
0
average savings rate per claim for Clinical Chart Review
0
average savings rate per claim for DRG Validation
Our relationship with Zelis has given us the flexibility to create customized solutions and bring value to our clients. The solutions and expertise that Zelis brings to the table, as well as its team’s ability to develop ideas to improve our processes, have created a mutually beneficial relationship for both our companies.
Our team recommends Zelis to any third-party administrators that are seeking a partner that will help them deliver superior service, provide strong cost reduction solutions, and continually looks for ways to improve its products and services.
Zelis has always given us the tools we needed to succeed. Working with their team has helped us navigate the constantly changing demands of the market that are generated by our clients’ needs, regulatory issues, and the passage of new legislation. We have a level of confidence that when something new comes up, we’re going to work with Zelis to solve the problem.
Request a Meeting
Let’s talk about modernizing your business.
There’s no shortage of ways we can help. Get a conversation going with one of our Solution Advisors and build a thoughtful approach aligned to your business goals.
Not what you were looking for?



