We’ve heard a lot about machine-readable files (MRFs) this year. Thanks to the Transparency in Coverage rule (TiC) that requires health plans to publish MRFs containing pricing information for in- and out-of-network items and services, almost everyone in the industry has been inundated with data, compliance, and how to handle the influx of it all. That’s no easy feat, often made even more aggravating by the reality that many don’t understand how all this data can be used to their advantage.
We understand the frustration health plans and providers alike are facing: You have data at your fingertips, but you have no avenue in which to use it. And you’re overwhelmed by the mere thought of doing something with it! Still, we shouldn’t ignore its great potential. MRF data can transform the healthcare industry, if used correctly.
On its own, MRF data, which includes a health plan’s in-network provider negotiated rates for all items and services, is a mass of data and numbers that mean very little to anyone, even to experienced industry stakeholders. But by pairing it with demographic data, for example, it becomes something usable and actionable, providing health plans with valuable competitor insight that can help lower costs. This data can also provide consumers and providers with estimated out-of-pocket costs.
Solving our biggest MRF challenges.
While it’s true MRF data can help shape the market and lower healthcare costs, we must first navigate the challenges associated with establishing compliance, as outlined by the Center for Medicare and Medicaid Services, and TiC price transparency tools.
Compliance is the biggest pain point by a landslide. As most of you know, this data must be posted monthly. It must be free and provide unfettered access, and you can’t limit your competitors’ access. Finding a way to pull all that off every month can be a tremendous challenge.
Then there’s the need to develop a member-facing price transparency tool. The goal is to enable members to get this information quickly. The MRF data must be accessible and posted via an Internet-based tool for members to access. When they do use this tool, the information they search for must be returned quickly.
The last obstacle health plans face? All your competitors can see this data and use it to their advantage. There are a lot of health plans that find this information extremely valuable as it relates to provider contracting efforts and new geographic markets to pursue. For example, providers and health plans can use it to think about how their competitors are being paid and where they sit in the pecking order as it relates to their negotiated rates.
In fact, providers are becoming increasingly interested in leveraging data to negotiate better rates and gain more knowledge about the negotiation process. Proof that health plans and providers alike have something to gain from MRF data.
Turning messy MRF data into actionable insights.
As I mentioned earlier, the data itself is not fully usable on its own. Although highly valuable, there’s very little identifiable provider information. It needs to be complemented with other provider demographic data to make it usable. That’s why it’s crucial that health plans ensure their partners have access to the right data to transform something very messy and complicated into something actionable.
Take this hypothetical scenario, for example: You’re looking for areas to lower costs, so you decide to evaluate rates for specific high-volume codes in one of your most competitive geographies. You start by focusing your analysis on that geography and look up one specific code. When you do, you find that your median rate of $37,000 is a shocking $21,000 more than your biggest competitor, who has a median rate of just $16,000 for the same code.
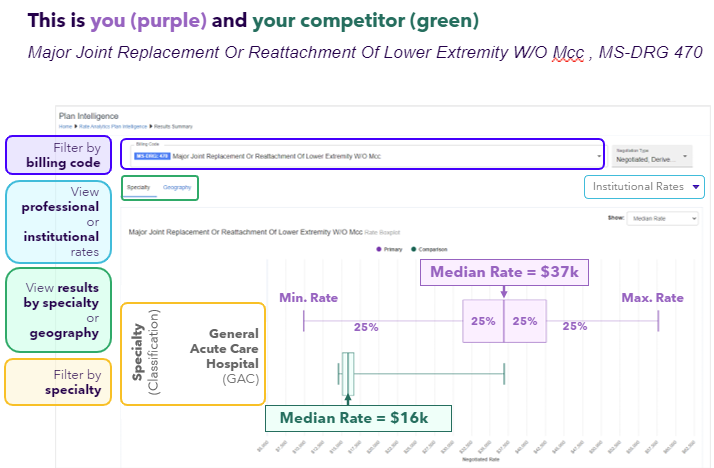
Let’s go back to our ninth-grade algebra classes for a second and do some quick math. By those calculations, if a facility performs just 50 procedures a year for $21,000 less, you could save a little more than $1 million. That’s a million dollars in savings for one procedure just by analyzing the right data! When we talk about the tremendous opportunity with MRF data, this is what we’re talking about. In this scenario, demographic data was added to focus the analysis on the geographic area and specialty of interest.
Leveraging utilization analytics.
Healthcare costs are soaring, and we all want ways to lower those costs where we can. That’s where healthcare utilization analytics with MRF data plays a pivotal role in helping uncover the aggregate financial implications of network contracting decisions.
Using MRF data as a framework, you can identify excessive spending, implement cost-saving measures, and optimize resource allocation. Utilization analytics can even support repricing across different healthcare payer networks, employer groups and providers, places of service, or geographies. It enables benchmarking and performance comparison too.
This is exactly why it’s important to look beyond the large amount of data and see it as a tremendous opportunity for your company. This is a game-changer for the healthcare industry. Think about all the benefits of repricing support or cost analysis. Choosing to invest in MRF data now positions you for success as the healthcare industry continues to evolve. And if you’re not using this data effectively to drive change in the market, you can be sure your competitors are.
Preparing for the future.
CMS will continue refining these regulations, and we can expect the requirements to evolve. Even just recently, CMS announced it would end the enforcement deferral period for prescription drug MRFs.
In other words, data sets are going to change in certain ways. Make sure you’re prepared to do more than just address them. Make sure you’re ready to take advantage of them too.
There are a lot of great resources out there to help you get started, and our team is happy to provide some guidance as you figure this out.




