Combining technology and human expertise can be an effective way to address payment integrity. But how exactly do you do that?
Here are some practical dos and don’ts to strengthen your bill review process.
Do: Use technology to automate manual and/or repetitive tasks.
This ensures your team and vendor partners can focus on what they do best by letting go of the monotonous administrative tasks that come with the job.
Don’t: Rely on automation and artificial intelligence (AI) alone.
As tempting as it may be, don’t rely solely on AI to process every single claim review. Each claim is an individual patient story. Those stories shouldn’t be completely automated. You need real people – clinicians and expert coders – reviewing them to catch missing information in that story.
And, worth noting, there is still a margin of error with these emerging technologies that can leave you at risk. Using a combination of both gives you a buffer.
Do: Use itemized bill reviews on high-dollar claims.
Conducting line-by-line reviews on high-dollar claims, where the reimbursement methodology is appropriate, is a great way to strengthen your payment integrity program. Often called itemized bill reviews, these types of reviews dive into the coding of the bill and ensure it adheres to all industry-standard billing practices and specific client-driven policy requirements.
Don’t: Underestimate the value of clinical chart review.
In addition to line-by-line reviews, clinical reviews offer an additional layer of value.
An article featured in Fierce Healthcare highlights the large amount, $31.2B, that traditional Medicare paid out in improper payments in 2023. The agency noted that the improper payments represent potential overpayments or payouts that were made despite a lack of information. A shocking 68% of payments lacked documentation to support the claim.
A clinical review includes a comprehensive review of complex claims conducted by a team of clinicians leveraging medical record documentation. These reviews ensure the clinical accuracy of billed charges that target advanced levels of care, experimental and investigational procedures, and specialty niche claims such as high-cost drugs and implants.
Take advantage of the benefits of clinical chart review to ensure proper documentation and accurate payments for each claim.
Do: Leverage integrated workflows.
Integrated workflows, including transfer of claims data and files, reduces the opportunity for human error and inefficiencies.
If you have manual workflows, what process do you have in place when the person responsible for manually sending claims files is out on PTO or an unplanned absence?
This seems obvious – people go on vacation all the time! – but it often falls through the cracks. Then someone heads for a weeks-long vacation and leaves thousands of dollars in unidentified savings potential, causing downstream detriment to both the member and payer.
If you do have a manual process in place, make sure it’s well-documented.
Don’t: Use only one review methodology.
Leverage multiple review methodologies, whether that’s a claims editing review or a comprehensive bill review.
By using multiple review methodologies that cover a vast array of claim types, sizes and provider types, payers are able to secure more savings, which in turn helps reduce the amount of waste in the system.
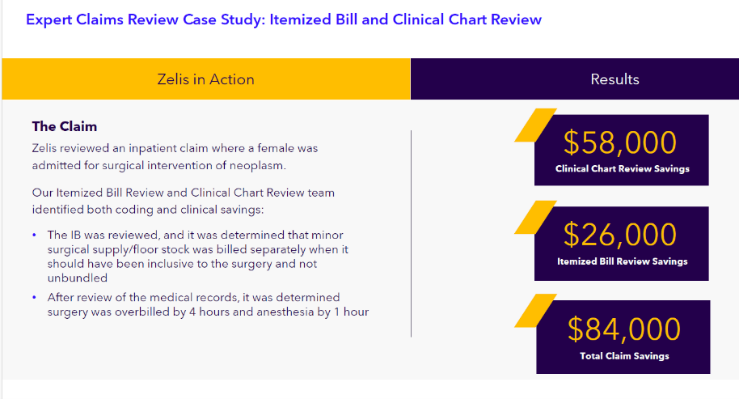
In the below case study, for example, a Zelis client saved $84,000 by leveraging both clinical chart review and itemized bill review. Without multiple review methodologies, their savings would have been significantly less.
Reducing waste and inaccuracies in billing and reimbursement will ultimately go toward investments in operations, benefit structure and member-facing solutions.
Do: Tackle high-dollar complex claims by using both AI and healthcare experts.
This combination ensures operational efficiency and an in-depth review by experts who have been on the front lines or are certified coders aware of your plans policies. They essentially become an extension of your organization.
These comprehensive reviews see the claim for what it is, a unique patient story that doesn’t always fit the textbook treatment or protocol.
If you need assistance with bill review, our team has developed a comprehensive solution, Expert Claims Review, that can help. Learn more here.



