Unlock Savings with Member-Centric Reference Based Pricing
Give control back to your members by setting maximum reimbursement amounts using pre-defined prices to provide a controlled savings reference-based pricing plan.
Why Zelis?
Increase healthcare plan savings with a focus on member empowerment
Zelis Open Access Pricing®, a reference-based pricing (RBP) solution, sets maximum reimbursement amounts using pre-defined prices. This cost management model gives members more control over their healthcare provider choices. Improve accuracy and reduce frustration with a technology-enabled way to load and manage contracts, apply real-time edits and regulatory updates, and reprice medical healthcare claims.
Key Points
- 2MM+ reference-based pricing claims repriced annually.
- 60,000+ EE lives.
- 97% retained savings.
- <4% member and provider inquiry rate.
- 25 years’ experience with provider negotiation, contracting and settlement.
- Direct provider agreements expand member access to care.
Unlock Healthcare Pricing Insights
With Zelis Price Map, you can unlock healthcare pricing transparency for Medicare hospitals by using aggregated CMS data to benchmark your plan’s Medicare reimbursement rate to the facility’s actual amount.
Explore Price MapOpen Access Pricing Platform
Set limits on rising healthcare costs while removing PPO network limitations.
Empower members to maximize plan benefits through comprehensive and customizable solutions. Our member-first reference-based pricing advocacy program includes pre-service patient outreach, provider education, contracting support, balance bill resolution, legal escalation support, and litigation representation for balance bills.
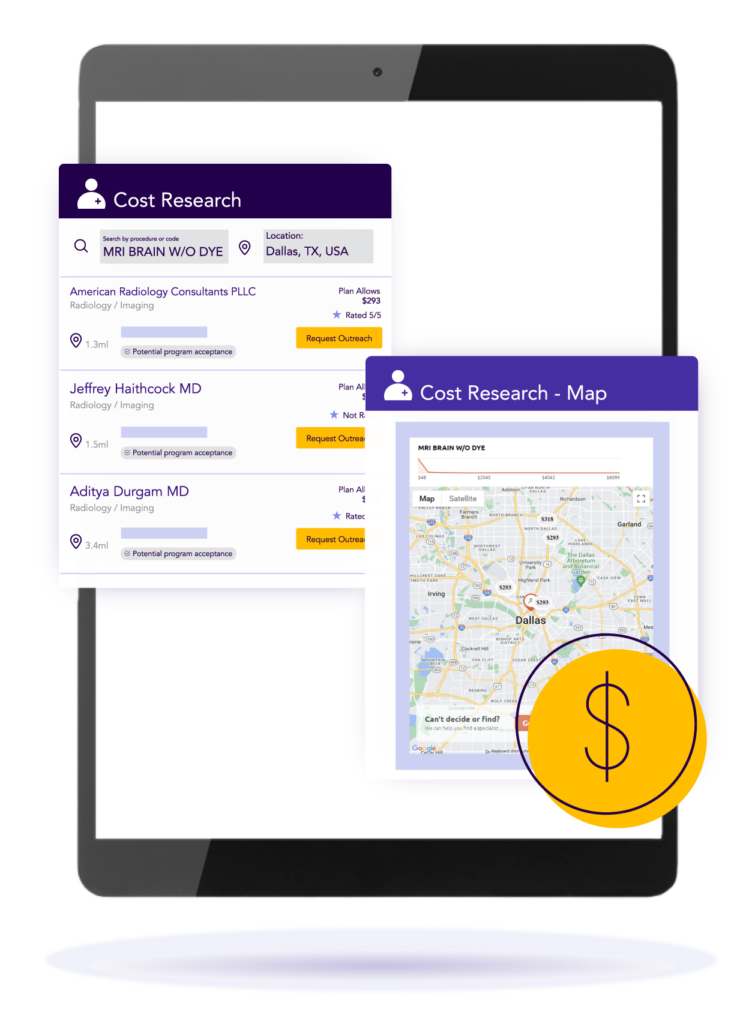
Drive enhanced health outcomes by empowering members with access to provider price and quality data. Zelis reference-based pricing plans drive member engagement with a decision-support app that provides convenient, timely access to essential provider information.
Members can find and compare providers by location, specialty, and service and compare cost and quality data. Plans love that they can guide members to high-quality providers who accept reference-based pricing plan rates.
Gain visibility into hidden reference-based pricing (RBP) insights to help your employer groups make more informed decisions before switching to Open Access Pricing.
Zelis Broker Connect is a free tool that leverages Zelis proprietary data to allow brokers to search for providers based on location, RBP acceptance status, and specialty.
Start gaining visibility into RBP-accepting providers in your region today to make better informed plan change decisions.
Zelis Open Access Providers℠ direct agreements expand provider access for reference-based pricing plans. These agreements include primary care physicians, clinics, hospitals, labs, and many other specialties.
Zelis’ direct provider agreements help plans reduce member abrasion by ensuring there are providers available to support reference-based pricing plan acceptance. The agreements help plans better predict plan costs and expected savings and minimize billing disputes.
Zelis Open Access Providers℠ offers a more robust reference-based pricing solution to help TPAs and brokers increase plan acceptance with groups who are typically less likely to consider alternatives to traditional PPO networks.
Zelis’ member-centric reference-based pricing solution supports members throughout their healthcare journey. In addition to our comprehensive member advocacy program Zelis also partners with Southern Health Lawyers, LLC (SHL) law firm to review plan documents for compliance and provide litigation representation.
Zelis has a wonderful staff with whom we’ve enjoyed working with over the last seven years. They’re responsive to our unique needs as a customer and always bring innovation and creativity, reaching out to us with new and exciting opportunities.
Zelis truly puts their money where their mouth is. They understand the value of partnership, and that everything in this business is driven by relationships.

Ready to control plan costs and empower members?
There’s no shortage of ways we can help. Get a conversation going with one of our Solution Advisors and build a thoughtful approach aligned to your business goals.
Connect with usTop Resources for Reference-Based Pricing
Blog

Making Strides Towards Healthcare Affordability: Insights from our Reference-Based Pricing (RBP) Survey
Reference-based pricing is a promising solution to overcome rising healthcare costs. But are brokers and TPAs using it to its full potential?
View resourceBlog

Debunking Common Reference-Based Pricing (RBP) Misconceptions
While it may seem straight-forward, there are still quite a few misconceptions about RBP. Get the facts in our latest blog here.
View resourceBlog
Reference-Based Pricing (RBP): An overview
Many struggle to afford the care they need. As such, it seems almost inevitable that an RBP model would emerge as a much-needed solution.
View resourceFrequently Asked Questions from Providers
We know reference-based pricing can feel unfamiliar—and at times, frustrating. Our goal is to make the process easier to understand, more transparent, and more respectful of your time and expertise. Below you’ll find answers to common questions from providers like you.
Reference-based pricing (RBP) is a method used by some health plans and third-party administrators (TPAs) to determine claim reimbursement based on a percentage of a benchmark—commonly Medicare rates or other publicly available data—rather than traditional PPO-negotiated rates.
We support health plans that use RBP to drive affordability and transparency, but we also recognize that it may differ from what you’re used to. Our role is to support plan design by pricing claims using rates that align to the plan’s custom reimbursement parameters.
Unlike PPO plans that rely on pre-negotiated contracts, RBP plans reimburse providers based on established benchmarks. That means there’s no traditional network agreement in place.
We serve as a pricing partner to the payer. That said, we’re deeply conscious of how these differences affect your practice, and we’re here to help bridge the gap with transparency, communication, and support.
Because RBP plans don’t require a contracted provider network, you may not receive prior notice of the plan’s reimbursement approach. However, members covered under these plans are typically informed upfront and encouraged to share plan materials with their providers.
We encourage open dialogue and aim to support providers with clear claim documentation and accessible support with pre- and post-service member and provider advocacy when questions arise.
Zelis is a service partner for reference-based health plans. While we don’t determine the pricing benchmarks, we do recommend pricing in accordance with plan documents and reimbursement parameters.
Balance billing policies vary based on plan type, claim type, and state regulations. Some RBP plans allow balance billing; others include member protections that limit it.
We help facilitate this conversation by providing transparent pricing details and offering optional negotiation support when needed in accordance with plan policies, so providers and patients can avoid unnecessary friction.
Our recommended pricing is based on independent, data-driven methodologies—often tied to Medicare benchmarks, customized plan specifications, or other fair market indicators. Each claim is reviewed using advanced technology and human oversight to ensure a balanced recommendation. We strive to deliver pricing that’s sustainable for payers, reasonable for providers, and supportive of member financial health.
We understand that sometimes our pricing may not align with your expectations. In those cases, we offer clear options:
Our goal is not to delay or deny payments, but to find a resolution that works for everyone involved—especially for the patient’s access to care.
The Explanation of Payment (EOP) or accompanying documentation includes contact information for provider support. Since we simply price the claim on behalf of the health plan in alignment with their reimbursement parameters, you’ll want to reach out directly to the health plan with any questions.
For questions about eligibility or prior authorization, please contact the TPA or health plan listed on the member’s ID card. We focus on pricing support, but we work closely with our payer partners to ensure a connected, coordinated experience.
If you ever have trouble identifying the right contact, we’ll do our best to point you in the right direction.
We believe your relationship with the patient comes first. That’s why our member-centric solution is built to minimize patient confusion and provider burden.
Our goal is to help patients afford the care they need without putting you in a difficult position. We’re committed to supporting health plans deliver accurate pricing, open communication, and real-time expert support to keep your focus where it belongs—on care, not claims.

