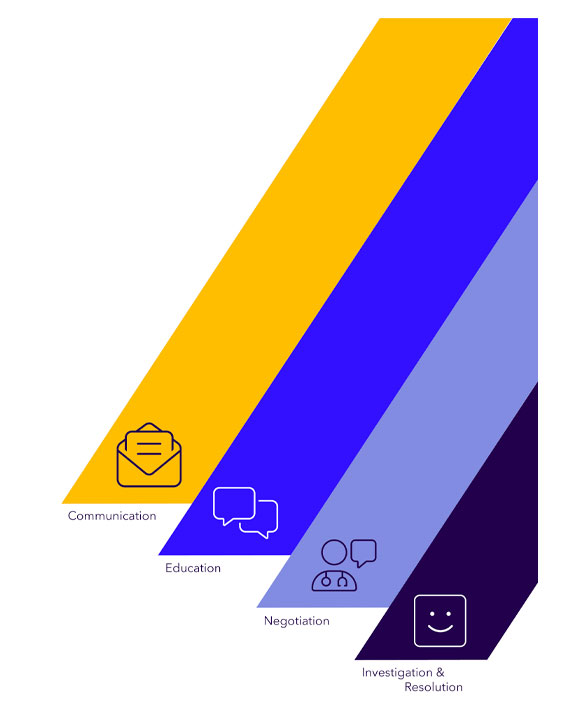
Clear communication & education
We take a proactive outreach to ensure members receive crucial information when out-of-network claims are processed. Our experts explain healthcare claims, the impact out-of-network services, and billing nuances related to plan benefits.