From $156K to $430: A Health Bill Win That Earned Member Trust
Member bill support from Zelis not only reduced a massive out-of-network health bill to just $430 – it earned one national plan lasting member loyalty.
When a health bill turns into a nightmare
A member of a national health plan received a shocking health bill: $156,000 in charges after their No Surprises Act (NSA) claim was denied — twice. The reason? Missing documentation, including an itemized bill and additional medical records. Despite the member’s efforts, the provider continued to pursue the full billed charges.

Solving the healthcare billing puzzle — one document at a time
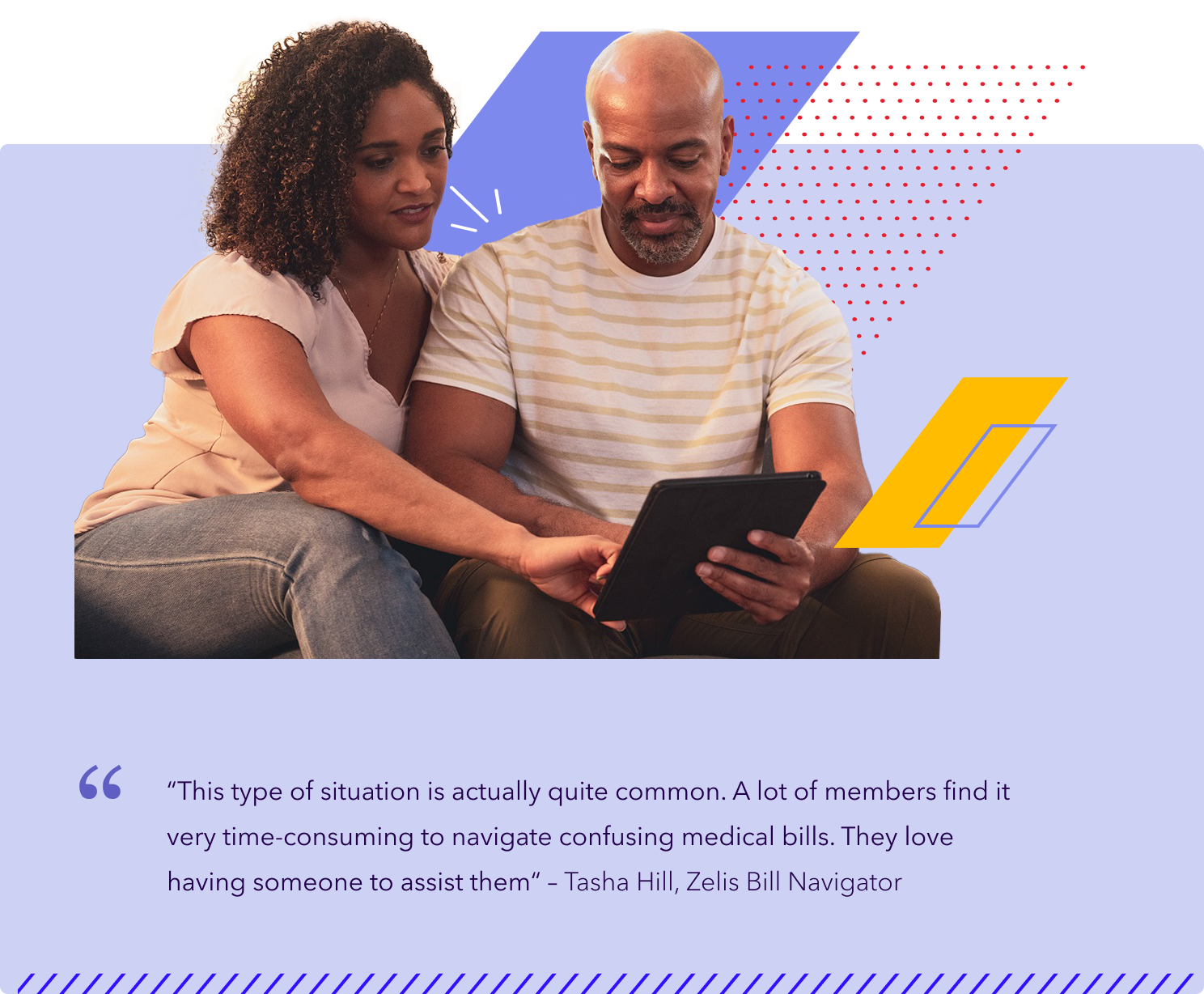
That’s when the member turned to Zelis Health Bill Assist® for help. Zelis Bill Navigator Tasha Hill quickly stepped in to help resolve this problem for the member. She researched provider contacts, coordinated with the health plan and gathered the necessary documentation.“The assuring thing was that I had an actual person that gave their number and always asked if I needed anything at all. Everything that Tasha said she was going to do, she did, which can be rare these days.”
— National Health Plan Member
From denied to approved: A healthcare billing win
The entire process took months to complete, but Tasha not only pursued the case, she even committed to seeing it through until the claim was completely reprocessed and accurately reflected on the member’s updated bill. The result? The provider adjusted the member’s bill from $156,000 to just $430.47.
Thanks to Zelis, the member avoided a stressful financial burden, the provider got paid faster and the health plan avoided a potential escalation.
Here’s what changed
- Original out-of-network bill: $156,000
- Final member responsibility: $430.47
- Member savings: $155,569.53
- Time to resolution: ~3 months with consistent follow-up from Zelis’ Bill Navigator
Contact us“The provider facility was really willing to work with me. From the beginning, they were appreciative and were very open to the questions I asked and the information I needed to assist with resolving this claim.”
— Tasha Hill, Zelis Bill Navigator
A healthcare billing solution that builds trust and delivers results
Denied claims and surprise out-of-network medical bills create confusion, stress and financial hardship for members. With Zelis Health Bill Assist, health plans can offer more than just support — they can build trust and loyalty.
Our team of Bill Navigators works behind the scenes to:
- Educate members on their out-of-network benefits
- Resolve complex billing issues
- Coordinate with providers and payers
- Facilitate accurate documentation and timely claim reprocessing
- Advocate for fair outcomes on behalf of members

Together, we can simplify the
out-of-network bill experience
When members face challenges with out-of-network health bills,
Zelis is ready to offer support. Let’s talk about how Zelis
Health Bill Assist can help your plan and your members.
Related Resources
Case Studies

Zelis Health Bill Assist℠ helped cut $52,000 in medical costs
Discover how to overcome confusing health bills. A member saved thousands with Zelis Health Bill Assist’s expert navigation.
View resourceCase Studies

How one health system manages high payment volume in half the time
See how one large health system cut payment reconciliation time in half and streamlined high-volume payments with Zelis.
View resourceCase Studies

From $156K to $430: A Health Bill Win That Earned Member Trust
See how Zelis Health Bill Assist® saved the day on a member’s $156k out-of-network medical bill.
View resource